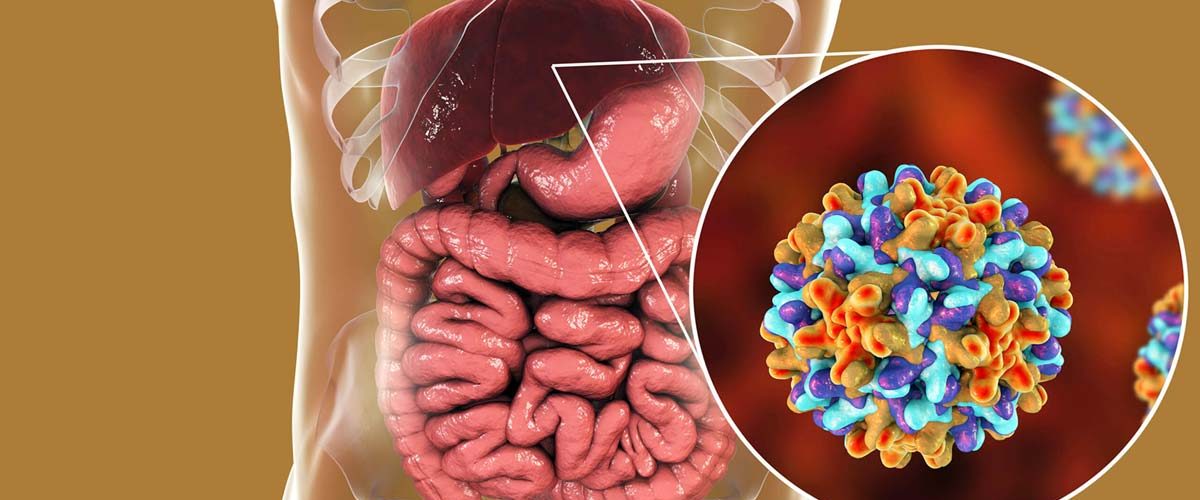
A variety of drugs has been introduced in the past to prevent, control and treat hepatitis B infection across the world. As time passes, the scientist report mutation in the viral genome, which reduces the effectiveness of the drug to counteract the infection. A study published in The Journal of Infection in the Developing Countries presented the latest research on the characteristics of the mutant form of HBV and its correlation with clinical outcomes.
Currently, there are 5 approved Nucleoside and nucleotide analogs (NAs) for the treatment of HBV in China which include lamivudine (LAM), adefovirdipivoxil (ADV), entecavir (ETV), telbivudine (LdT), and ten of ovirdisoproxil fumarate (TDF). Among these, ETV is considered the most potent antiviral with high potential to act against resistance form. Hence, it is recommended by many clinicians as the first line of defense. However, some use LAM and ADV along with ETV for long term prescription.
The lead author, Jinman Shao, identified that few of the patients incoming in the hospital set up developed resistance against the standard treatment, Adefovir plus entecavir (ADV+ETV) rescue therapy with chronic hepatitis B virus (HBV) infection in ETV-resistant patients.
He reported, “Thirty-seven ETV-resistant patients were requested to participate in the survey, which revealed twelve patients with an inadequate virological response to ADV+ETV rescue therapy.”
The team explained, “ETV-resistant mutants were identified in 10 of the 12 patients, whereas rest of the patients were diagnosed with multidrug-resistant (MDR) mutants, including a novel strain (rtL180M+A181V+T184A+S202G+M204V). Moreover, 7 out 12 patients completely recovered after the therapy; however, among 4 patients the viral mutants converted into a wild type of virus, which can prove to be harmful.”
Thus, for the first time ever, this study pointed out the risk of MDR HBV mutation for the ADV+ETV combination therapy in ETV-resistant leading to poor efficacy of treatment.













Add comment